Recently, ZUMA-7 study patients with early relapsed LBCL (<12 months after first-line immunochemotherapy) who were treated directly with CAR T-cell therapy in second-line instead of third-line, had a significantly better overall survival (OS) compared to patients who were treated with standard salvage treatment consisting of high-dose chemotherapy followed by autologous stem-cell transplantation (HDT-ASCT). Despite non-protocolled cross-over to CAR T-cell therapy in third-line for 57% of patients in the HDT-ASCT arm, a significant difference in OS of 9% remained, suggesting that patients benefit if the most effective therapy is applied at an early stage.
On the basis of these results, the paradigm of HDT-ASCT shifted to CAR T-cell therapy as second-line therapy for patients who have refractory or early relapsed disease <12 months. However, patients with a late relapse (>12 months) are still unable to receive CAR T-cell therapy until the third-line. A main argument is that late relapsed LBCL is considered to be still chemo sensitive and therefore these patients would have a better OS following HDT-ASCT salvage. The aim of this study was to compare the responses of LBCL patients with an early (<12 months) versus a late (>12 months) relapse onset, to see whether this argument is justified in real world.
All patients diagnosed with LBCL between 2005 and 2020 in the province Friesland, The Netherlands, were included (n=877). Detailed patient characteristics and outcomes of patients in first-line, relapsed setting and beyond were analyzed. OS was calculated from relapse onset.
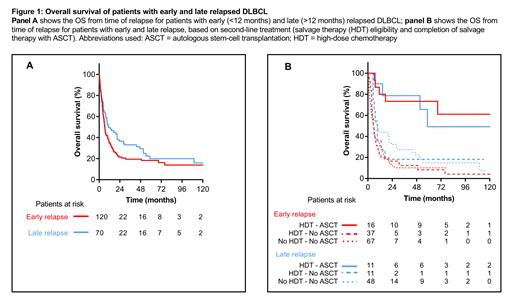
Median follow-up was 7.0 years from diagnosis (range 0.01-15.6). In the first line, 729 patients (83.1%) were treated with curative intent. Early relapse (refractory and <12 months after first-line therapy) and late relapse (>12 months) occurred in 120 (16.4%) and 70 patients (9.6%), respectively. Patients with an early relapse show a 2-year and 5-year OS of 21.5% and 18.3%. Compared to early relapse, patients with a late relapse show a slightly favorable OS of 36.1% at 2 years, yet an almost similar OS at 5 years of 19.6%. Main cause of death for both groups were lymphoma, including treatment related complications (93.9% in early and 82.6% in late relapse).
Second-line salvage therapy, consisting of HDT was initiated in 53 patients (44.2%) with early and 22 patients (31.4%) with late relapsed disease. Of these, only 16 patients (30.1%) with an early relapse and 11 patients (50%) with a late relapse obtained a sufficient response and maintained an acceptable clinical performance to undergo ASCT. Patients who completed ASCT, had a 5-year OS of 73.3% (early relapse) versus 49.2% (late relapse). In contrast, early and late relapsed patients who initiated salvage HDT but did not reach ASCT showed a 5-year OS of only 8.3% and 18.2%, respectively. This OS was comparable to the 67 patients (55.8%) with an early relapse who were upfront ineligible to start salvage HDT (5-year OS 10.2%). For HDT-ineligible patients with a late relapse (n=48, 68.6%) OS was similarly disappointing with a 5-year OS of 14.6%
In conclusion, these real-world data contradict the argument that LBCL patients with a late relapse (>12 months) have an advantage over patients with early relapse (<12 months) in their potential to reach a long-term remission and survival with HDT-ASCT. This supports the evaluation of early application of CAR T-cell therapy in second-line, also for DLBCL patients who relapse beyond 12 months.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal